Deion Sanders Shares Journey with Bladder Cancer and Neobladder Reconstruction
Guest Contributor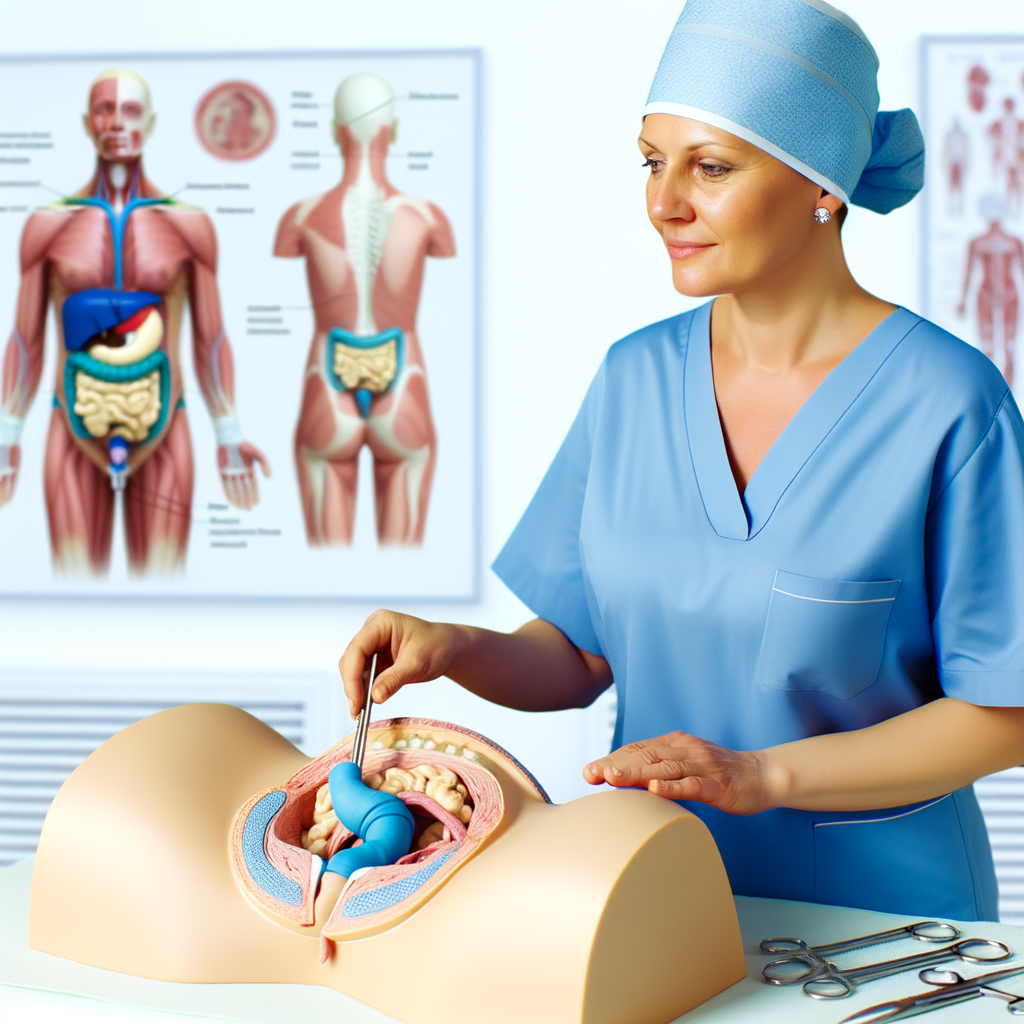
When Deion Sanders stepped up to the microphone at a recent press conference, he wasn’t just speaking as a football coach or a two-time Super Bowl champion. He was speaking as a survivor. The University of Colorado head coach shared his experience with bladder cancer and the remarkable surgery that gave him a new lease on life — and a new bladder. His story sheds light on a lesser-known but life-changing procedure called neobladder reconstruction, a surgery that uses a patient’s own small intestine to build a replacement bladder.

Neobladder reconstruction is often used to treat aggressive forms of bladder cancer, the type Sanders was diagnosed with earlier this year. According to the American Cancer Society, an estimated 85,000 people in the U.S. will be diagnosed with bladder cancer this year. Most of them will be men, but women often face more advanced and aggressive forms of the disease, in part because early symptoms like blood in urine may be mistaken for menstrual bleeding.
Sanders’ tumor was found during a routine checkup. As he put it, if he hadn’t gone in for that appointment, “things might have turned out very differently.” That early intervention allowed his medical team to act quickly, performing a complex but increasingly common surgery that offers patients a way to live without relying on external urine collection devices.
The surgical process is both intricate and astonishing. Dr. Max Kates, codirector of the Greenberg Bladder Cancer Institute at Johns Hopkins University, described the steps involved in creating a neobladder. First, the original bladder is removed. Then, surgeons take about 18 inches of the ileum, the final section of the small intestine, and reshape it. One side of the intestinal segment is cut open so it can lie flat, then folded in half and sewn into a pouch. Kates likens the final result to a volleyball stitched together with sutures. This new bladder is then connected to both the kidneys and the urethra, allowing urine to pass through the body much like it did before.
What makes the neobladder particularly effective is that it’s built from the patient’s own tissue. Dr. Janet Kukreja, Sanders’ surgeon and director of urologic oncology at the University of Colorado Cancer Center, emphasized that this biological compatibility eliminates the need for immunosuppressant medications. Unlike plastic or synthetic materials, which the urinary tract would reject and which could lead to complications like bladder stones, the intestinal tissue integrates naturally into the body’s systems.
Kukreja performed Sanders’ surgery using a robotic, laparoscopic approach. This minimally invasive method involves small incisions and typically results in shorter hospital stays and faster recovery times. Most patients spend only a few days in the hospital post-surgery, though adapting to the new bladder takes longer.
One of the challenges of living with a neobladder is that it lacks the nerve signals that tell the brain when it’s time to urinate. Dr. Jodi Maranchie, a surgical urologic oncologist at UPMC in Pittsburgh, explained that patients must gradually train themselves to control their new bladder. Over time, they learn to extend the intervals between bathroom visits. Daytime continence is usually achievable, but nighttime leakage often remains an issue.
Sanders addressed this with characteristic humor during his press conference, noting that he now “depends on the Depends,” a nod to the adult incontinence products he uses at night. Far from being embarrassed, he used the moment to encourage others facing similar challenges to speak openly and seek support. “Let’s stop being ashamed of it,” he said. His candidness resonated deeply with many, including Dr. Kates, who told NPR he “loved every moment” of Sanders’ remarks. Kates noted that two of his own patients, both men around Sanders’ age, felt validated by the coach’s openness.
I found this detail striking — that the emotional impact of a public figure’s honesty could ripple through the lives of others facing the same condition. In a world where health issues are often kept private, Sanders’ willingness to speak publicly about his journey with bladder cancer and neobladder reconstruction not only demystifies the procedure but also helps reduce the stigma that can accompany it.
This kind of transparency is especially important given how subtle the early signs of bladder cancer can be. A single symptom — blood in the urine — may be easy to overlook or misattribute. Sanders’ story underscores the importance of regular health checkups and early detection. “Please get yourself checked out,” he urged. “Because if it wasn’t for me getting tested for something else they wouldn’t have stumbled up on this.”
Bladder reconstruction surgery is a testament to both medical innovation and the body’s resilience. While a neobladder doesn’t function exactly like the original, it offers patients a way to regain control and maintain quality of life after a cancer diagnosis. And thanks to minimally invasive techniques and the use of the body’s own tissues, recovery is often faster and smoother than many might expect.
Deion Sanders’ story is one of strength, science, and self-advocacy. By sharing his experience, he’s not only shedding light on an advanced surgical option but also encouraging others to prioritize their health and speak openly about their challenges. For many facing bladder cancer, that message may be just as life-changing as the surgery itself.

